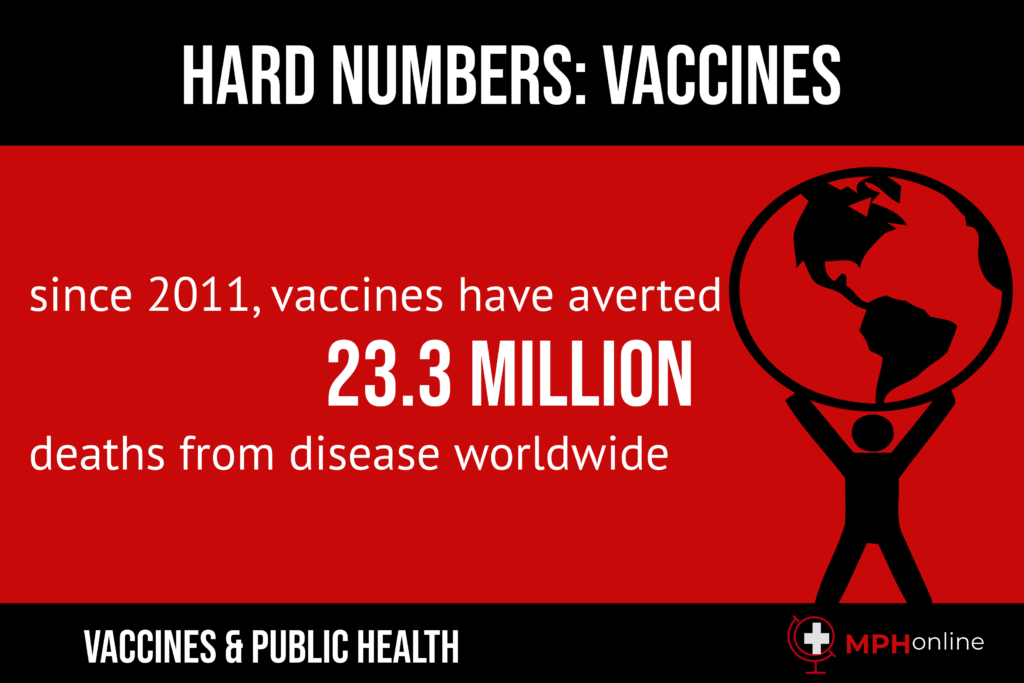
Vaccines are one of the triumphant achievements of the modern era. The ability to prevent diseases before getting them changed human life forever. The vaccine process protects recipients from bacterial or viral infections. Diseases that spread by viruses include smallpox and measles, while bacteria called Streptococcus pneumonia cause numerous diseases such as meningitis, pneumonia and sinus infections.
Have you ever wondered how vaccines are made?
The vaccine development process has saved hundreds of millions of people from getting sick or dying of illnesses. Today, we have eradicated smallpox and greatly decreased the occurrence of polio and measles. With the coronavirus pandemic, the world has been reminded of the importance of vaccines. However, many people don’t understand the vaccines manufacturing process.
The major stages of developing new vaccines include the following:
- Vaccine development process
- Vaccine testing process
- FDA approval process for vaccines
- Process of making a vaccine
The process of making vaccines is a complex and time-consuming endeavor.
How are vaccines made?
There are three basic ways to make vaccines for viruses. The virus vaccine development process consists of the following methods:
- Weaken the virus
- Inactivate the virus
- Use only a portion of the virus
How do scientists weaken a virus?
This process of making a vaccine involves weakening the virus so it cannot properly reproduce inside the human body. Many major vaccines use this method, including mumps, measles, rubella, rotavirus, influenza and chickenpox.
When viruses reproduce themselves, they cause havoc in the human body. Natural viruses can rapidly reproduce themselves, causing an infection. However, the viruses in vaccines may copy themselves just two dozen times. This is not enough to cause serious illness, but it is enough to cause an immune response that causes the body to make memory B cells, which protect against future infections.
The vaccine process development for live vaccines is designed to produce lifelong immunity. However, these vaccines don’t work with people who have compromised immune systems. That means that those with aids or cancer may have to go without this protection.
How are vaccines made when researchers inactivate the virus?
Let’s look at how vaccines are made by inactivating the virus. Using this method, researchers first kill the virus by chemical means. This means the virus cannot reproduce itself. The vaccines production process for this method includes hepatitis A, inactivated polio, rabies and the flu shot. The immune system reacts to the presence of these dead cells, causing immunity against future infections.
The process of making vaccines like this has two advantages. The recipient doesn’t even develop a mild case of the disease, and it is safe for people with compromised immunity. However, several doses are needed to achieve the desired result.
How are vaccines made using part of the virus?
Researchers isolate one part of a virus and make a vaccine that destroys it. This is how vaccines are made for the human papillomavirus and shingles vaccines. This vaccine methodology works when the immune system can act on one part of the bacteria or virus. This type of vaccine process works for those with weak immune systems after just two doses.
How are vaccines made using part of bacteria?
Bacteria cause disease by making a toxin. Researchers can create vaccines by inactivated toxins. Once the toxin becomes inactivated, it is known as a toxoid. There are several vaccines based on this method such as tetanus, pertussis and diphtheria.
A second way that researchers make bacterial vaccines involves the bacteria’s sugar coating. This is called a polysaccharide. Preventing infection depends on developing an immunity to the polysaccharide. Young children are at a disadvantage because they don’t have good immune responses yet. However, vaccines based on the sugar coating can be connected to harmless proteins too make effective vaccines for children as well as adults.
Similar to inactivated viral vaccines, these vaccines are safe for people with compromised immune systems. However, they also take several doses to get the desired immunity.
How does the vaccines development process work?
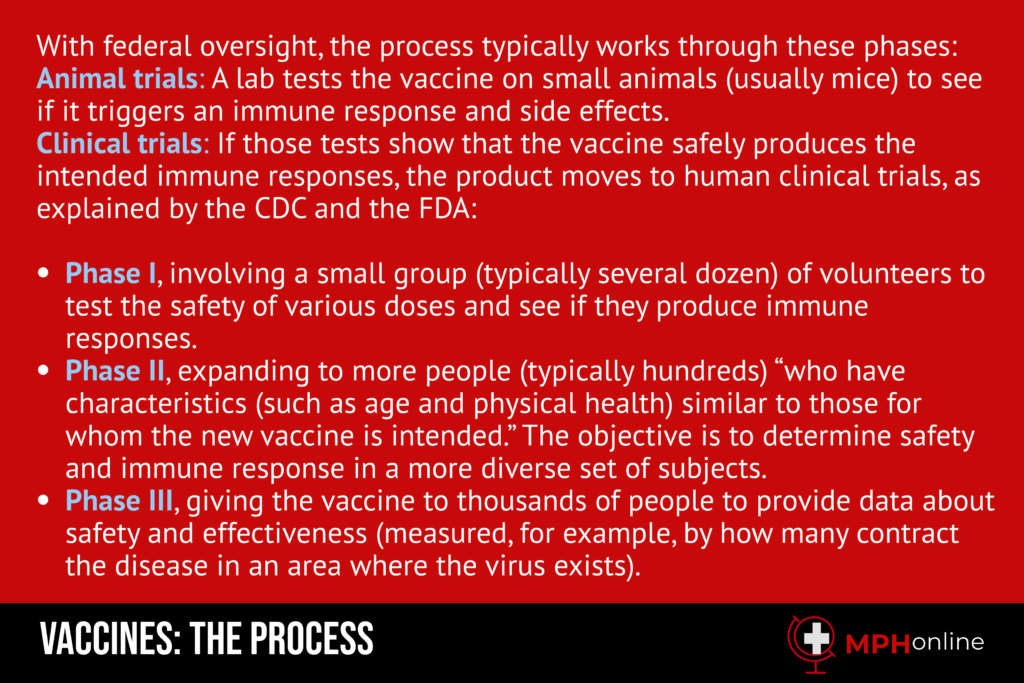
There are several stages to the development of new vaccines. Steps of the vaccine process development include:
- Exploratory
- Pre-clinical
- Development in a clinical setting
- Approval process for vaccines
- Manufacturing, if approved
- Quality assurance
This can be broken down into various phases. Let’s take a look at how each phase impacts how vaccines are made.
- Phase I: researchers give the drug to a small test group.
- Phase II: the study expands to include more people in the target range of the vaccine. This could include health, age and other factors,
- Phase III: At this advanced stage of vaccines development process, testers give the prospective vaccine to many thousands of patients to test for effectiveness and monitor side effects.
There is one more stage of testing in the vaccines development process. Not all drugs go through Phase IV, but those that do undergo ongoing studies as part of the FDA vaccine approval process.
Who handles the approval process for vaccines?
The vaccine process development includes formal approval by the US Food and Drug Administration. The FDA approval process for vaccines is very involved. Within the FDA, the Center for Biologics Evaluation and Research regulates the testing and approval of vaccines.
The vaccine approval process includes many steps. Sponsors of new vaccines must follow these steps precisely to avoid delays in the approval process.
- To start the vaccine approval process, sponsors fill out an Investigational New Drug application.
- Next, the manufacturers manage the pre-licensure vaccine testing process
- Sponsors fill out a Biologics License Application (BLA)
- The last stage involves the manufacturing process of vaccines. Inspectors visit and approve the manufacturing facility.
- If inspectors approve the vaccine manufacturing process, findings are presented to the Vaccines and Related Biological Products Advisory Committee (VRBPAC).
How is the vaccine manufacturing process regulated?
Once the vaccines production process advances to the vaccine manufacturing process, the next step is the final approval. However, the FDA vaccine approval process can sometimes take months or years.
The FDA vaccine approval process continues beyond the initial sign-off on a new drug. The vaccine testing process continues as the FDA monitors the production process, addressing any safety concerns. In fact, the monitoring process incorporates facility inspections that continue for the duration the manufacturer is licensed to create a particular vaccine.
The approval process for vaccines may include special requests for the manufacturing process. The FDA may add steps to the manufacturing process of vaccines to ensure the manufacturer has set up their own internal checks. As part of the manufacturing process of vaccines, drug companies must test batches for purity, potency and safety. This essential step of the vaccines production process must be completed for every lot of vaccines made.
Additionally, the FDA may require samples for each lot tested during the vaccines manufacturing process.
How does the vaccines development process handle product labeling?
The vaccines manufacturing process includes labeling the vaccines according to FDA regulations. In order to receive full FDA approval, vaccine manufacturers have to provide appropriate product labeling. This allows health care providers to interpret the use and effectivity of the vaccine. It may also include instructions on how to administer the vaccine.
Product labeling for vaccines and other drugs include the risk and benefits of receiving the vaccine. The vaccine process is designed to communicate the information that parents need to make informed decisions about their children’s health.
The APLB handles the advertising and labeling side of the vaccine approval process. This involves both regulating and evaluating how manufacturers advertise and label the vaccines.
CBER products require specific advertising parameters and contents on the labels. This ensures that the public remains well-informed regarding the risk that may be associated with using the product. The APLB ensures the truthfulness and scientific basis of claims made in advertising and instructions and information provided on the labels. It also ensures that the vaccine manufacturer follows relevant federal laws.
The APLB evaluates proprietary names to ensure that they do not imply or misrepresents the function of approved drugs. They also look for medication errors that can affect the proper administration of the vaccine.
What about a vaccine for COVID-19?
Scientists are trying to streamline the process for developing a COVID-19 vaccine. The process needs to go quickly in order to prevent more deaths on the national scale and to put a halt to the pandemic that has already claimed hundreds of thousands of lives.
In order to make things move faster, several stages are happening at the same time. This requires a huge influx of capital with no guarantee that the investment will pay off. Typically, scientists have to ask for funding and show that their results warrant further testing and development. Much of this is being streamlined in order to get as many ideas on the table as possible.
When it comes to defeating the novel coronavirus, all bets are on the table. It’s as if the FDA has opened up the racetrack and is betting on all the horses to ensure that any winners pay off.
For researchers, this means preparing for clinical trials at the same time production facilities are ramping up in readiness for large scale phases as well as future deployment of the vaccine should it improve effective.
Related:
Preventative Care and Public Health
Best Practices During a Pandemic
A Comprehensive Pandemic Survival Kit List
What’s the Difference Between a Virus and a Syndrome